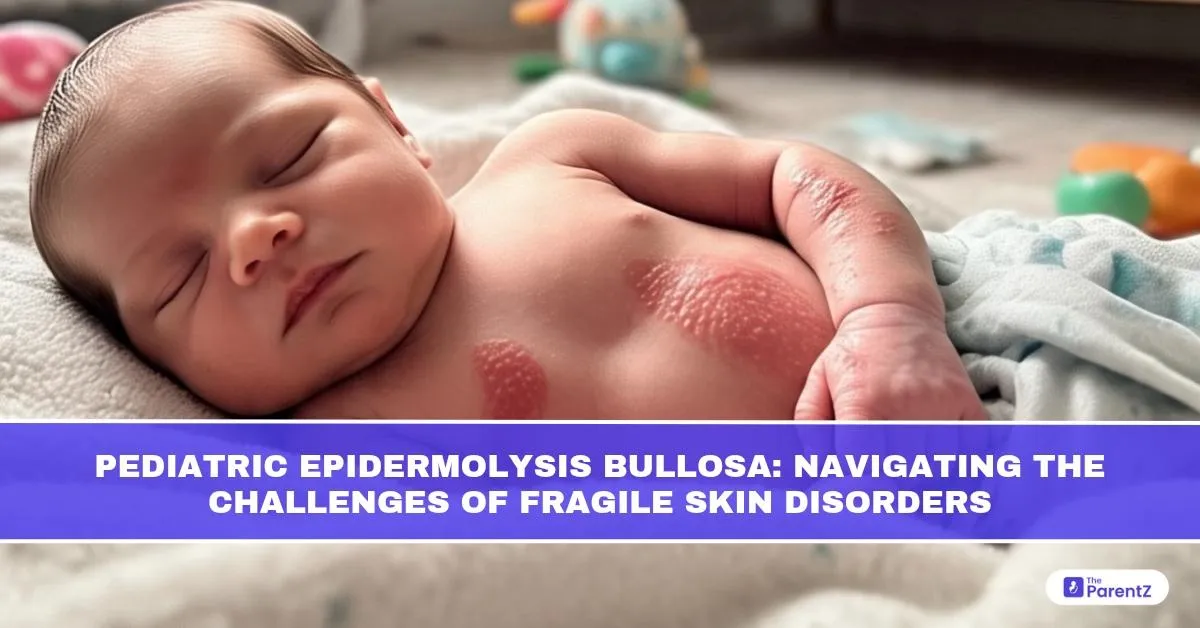
Imagine a world where even a gentle hug, a bandage, or a pair of shoes could tear the skin. This is the reality for children living with Epidermolysis Bullosa (EB), a group of rare genetic conditions characterised by fragile skin that blisters easily in response to minor friction or trauma. Though the appearance of EB can be startling, understanding its origins, classifications, and care strategies can offer hope and comfort to families navigating this lifelong condition.
What is Epidermolysis Bullosa?
Epidermolysis Bullosa refers to a genetic skin disorder in which the skin’s layers, the epidermis (top layer) and dermis (underlying layer), fail to adhere properly. The defective connection leads to skin separation, forming painful blisters, sores, and in severe cases, deep wounds.
EB is not a single disease but a group of disorders that share this underlying problem of skin fragility. Symptoms can range from mild skin issues to widespread blistering that affects internal organs and severely impairs quality of life.
Is EB a Disease or a Disorder?
EB is best classified as a genetic disorder. The underlying issue stems from mutations in genes responsible for skin integrity. Depending on the gene affected, different types of EB emerge, each with varying degrees of severity and clinical challenges. While it causes disease-like manifestations, the core cause remains a heritable defect, making it more accurately a disorder than an acquired disease.
What Causes EB?
EB is caused by mutations in genes that encode proteins responsible for the structural integrity of skin and mucous membranes. These proteins help bind the epidermis and dermis together. When these proteins are absent or dysfunctional, even the slightest friction can cause the layers to separate.
The disorder follows different inheritance patterns:
- Autosomal dominant in milder forms (e.g., EB simplex)
- Autosomal recessive in more severe types (e.g., recessive dystrophic EB)
If both parents are carriers in recessive forms, there’s a 25% chance of the child being affected in each pregnancy.
Types of Epidermolysis Bullosa in Children
EB is broadly categorized based on the skin layer where the blistering occurs:
- EB Simplex (EBS): Blistering occurs in the upper epidermis. Usually milder, with localized blistering on hands and feet. Normal wound healing and less scarring.
- Junctional EB (JEB): Blisters form in the basement membrane zone (between epidermis and dermis). More severe, may involve mucous membranes. Risk of respiratory and feeding issues.
- Dystrophic EB (DEB): Blistering occurs below the basement membrane. Associated with chronic wounds, scarring, and fusion of fingers and toes. Can lead to disfigurement and impaired mobility.
- Kindler Syndrome: Rare form with mixed blistering levels Includes skin fragility, photosensitivity, and early aging of skin.
The severity varies not just between types but also within each type, depending on the specific genetic mutation.
When and How Does EB Present in Children?
In most cases, symptoms are evident at birth or within the first few weeks of life. Some forms, particularly milder variants, may go unrecognized until a child begins crawling or walking.
Common signs in newborns include:
- Blisters from birth or shortly after
- Raw or eroded skin in pressure areas (e.g., joints, back of head)
- Blisters in the mouth, eyes, or diaper area
- Delayed healing or frequent wound recurrence
As children grow, they may develop:
- Scarring and skin discoloration
- Nail loss, hair thinning, or dental issues
- In severe cases, growth delay, nutritional deficiencies, and esophageal strictures
Diagnosis and Genetic Testing
Diagnosis begins with a careful clinical evaluation, followed by skin biopsy for immunofluorescence mapping to determine the level of blistering. This test helps differentiate EB subtypes based on where the skin splits.
Genetic testing is essential to confirm the diagnosis, understand the specific mutation, and provide accurate genetic counseling. Prenatal testing may be offered in families with known mutations.
Management: Supportive and Specialized Care
There is currently no cure for EB, so treatment focuses on symptom management, wound care, and preventing complications. Each child requires an individualized care plan involving multiple specialties.
Key aspects of management:
- Wound Care
- Pain and Itch Management
- Nutritional Support
- Mobility and Physical Therapy
- Psychosocial Support
Complications of EB
Children with severe EB may face multiple systemic complications:
- Anemia due to chronic blood loss from open wounds
- Infections, including sepsis
- Malnutrition from poor oral intake
- Esophageal narrowing, making swallowing difficult
- Fusion of digits (syndactyly) due to repeated scarring
- Aggressive skin cancer (SCC) in adolescence or early adulthood, especially in DEB
These complications underscore the need for lifelong monitoring and coordinated care.
Advances in Treatment and Hope for the Future
Research is ongoing, and several promising therapies are in development:
- Gene therapy: Trials are exploring the delivery of corrected genes directly into skin cells.
- Protein replacement therapy: Investigates supplementing missing structural proteins.
- Stem cell transplants: Aimed at regenerating healthy skin layers.
- Topical gene-modified skin grafts: Under clinical trials for localized healing.
Though these treatments are still experimental, they bring hope for improved outcomes in the future.
Living with EB: Family-Centered Approach
Raising a child with EB is emotionally and physically demanding. Parents often become skilled caregivers and wound care experts. Empowering families with education, home care training, and access to multidisciplinary teams can reduce hospital visits and improve quality of life.
Children, with the right care, can go to school, make friends, and pursue creative passions. Awareness among educators, caregivers, and peers is key to creating an inclusive and safe environment.
Conclusion
Pediatric Epidermolysis Bullosa is more than a skin condition — it affects nearly every aspect of a child’s life. While the condition is rare and challenging, early diagnosis, gentle care, and family support can make a tremendous difference. The journey can be complex, but with growing awareness and advancing research, children with EB can live fuller, more comfortable lives.
References
- Fine J-D et al. Inherited epidermolysis bullosa: updated recommendations on diagnosis and classification. J Am Acad Dermatol.
- National Epidermolysis Bullosa Registry (NEBR)
- NHS Clinical Guidelines for Pediatric EB
- Indian Pediatrics – Rare Genetic Skin Disorders in Children
- Orphanet Journal of Rare Diseases – Advances in EB Research




Be the first one to comment on this story.